Assistive Listening Devices – Trust Me, They Work!
Issues in Accessibility
Janine Verge, AuD, Aud (C) is coordinating the “Issues in Accessibility,” column which will cover topics addressing issues in accessibility for people who are Deaf/deaf and hard of hearing.
Noise has been around a long time. The first noise was the big bang. The first reference to noise impacting society was documented in the 6th century Greek colony, ruling that potters and other tradesmen live outside city limits because of the noise they made.1 As a profession we have been trying to understand the impact of noise on our clients since our profession was born. In fact, it was the noise induced losses of the veterans returning from war that drove our profession into existence. Carhart investigated word recognition scores in sawtooth noise in hopes of deriving a test to help with hearing aids selection.2 And it continues to today. While often touted as a reason for rejection of hearing aids, the acceptance of the devices might not be solely related to the performance of speech in noise3,4 but rather, as Nableck et al.5 has demonstrated, the tolerance of the individual to the background noise itself. This led Taylor and Bernstein,6 to develop the red flag matrix as a method for assessing both speech in noise and acceptable noise levels to develop a better counselling tool for those with hearing difficulties.
It is not lost on the audiologist, that sensorineural hearing loss can impact hearing in noise performance, but its impact is not consistent. That is, similar audiograms can have very different speech outcomes.7 From an diagnostic audiology perspective, hearing in noise can be impacted by dysfunction anywhere along the auditory pathway from cochlea to temporal lobe,8 corpus callosum,9 insula,10 and the efferent auditory pathway.11–13 The term hidden hearing loss describes a condition with normal hearing sensitivity with hearing in noise difficulties.14 Research has suggested the spiral ganglion as the site of dysfunction of as a possible though hard to measure with current technology. Therefore, hearing in noise as a presenting symptom is not very telling. In addition to those with hearing loss, it is estimated between 12 and 29% of those adults with normal hearing have hearing difficulties.15,16 The nagging question is what to do with clients who suffer from this ubiquitous problem?
Due to the fact that a majority of real-world listening conditions most commonly range from −10 to +5 dB SNR, the speech recognition ability of people with sensorineural hearing loss is often at a disadvantage in background noise.17 Young children (6 years old) with normal hearing and adults with sensorineural hearing loss may require a SNR of greater than +15 dB for optimal speech recognition scores.18,19 While hearing aids continue to advance, the benefit they offer in noise is about 5–8 db SNR.20,21 Assistive listening technology has demonstrated value for both sensorineural hearing loss and clients with normal hearing complaining of hearing difficulties.22 Yet assistive devices are still not readily adopted.23
Kochkin has demonstrated that the uptake of assistive devices is about 1% in populations with hearing loss and noting that a small number, approximately 25%, only make use of their directional microphones or telecoils.24 This would appear to fly in the face of conventional thinking, how can something that we know works so well, find limited acceptance? Particularly since research has been demonstrated that undiagnosed and untreated hearing difficulties has such a huge impact on the individual,3,25 the family,26 and society as a whole.27,28 Untreated hearing loss has been linked to social isolation,29 depression,30 dementia,31,32 and may also hamper the ability of clients to participate in their own care.33
Certainly, cost is a factor but perhaps something much larger is threatening the uptake and that could be the manner in which we practice. Over the past 20 years there has been a shift from the medical model to one of chronic care and client focus. The medical model is clearly not working when hearing aid penetration is approximately 25%.34 Focusing on the service and expertise that our profession has to offer and directing the client towards achieving communication goals appears to provide better direction and support for the client.35 Different approaches to administration of audiological care is not new.36–41
However, change to clinical practice takes time. Westfall et al estimates on average it takes 17 years for 14% of research to be integrated into the routine clinical practice.42 While the reasons for this knowledge transfer gap is complex, if we can make subtle changes to our clinic practice, those that take several minutes but lead to improved client outcomes, the shift will be worth it. This seems to be supported by two streams of thinking. One method, Plan-Study-Act-Do, or PDSA, the other being client centred approach.
The PDSA cycle is a method in which there is an iterative process of testing changes to improve quality.43,44 According to Taylor et al, using small scale tests allows for flexibility and adaptability to ensure specific solutions are developed, minimizing risk and allows evidence of change to be gathered.44 Client centred care is a process of client engagement, establishment of communication goals and then guiding them forward to achieve those goals.35
There are standards and guidelines to ensure the best fit for assistive devices but this happens once the devices are purchased and ready to be fit. How can we give the client a glimpse of the potential benefits of such devices so they can make an informed decision? The medical model would say, “trust me I am the expert and I know FM system will work for you.” The client care model would script a goal about communication and then attempt to provide information that could potentially help the client.
Jerger and Hayes demonstrated a method to assist clients in determining how demonstrate FM system effectiveness.45 The step up for the procedure in the booth is relatively simple. Speakers are placed so that the client is seated directly in the middle of the two speakers, about one meter in front and behind the client. Using synthetic sentence materials, Jerger and Hayes set out to test a number of clients across a variety of signal to noise ratios (SNRs) from easy (+20) to difficult (−20).45 The stimuli utilized in the study consisted of material from the Synthetic Sentence Identification.46 The “noise” is the competing track of the test with Jerger telling the story of Davey Crokett and is set at 40 dB HL. When the test material is set at 40 dB, a 0 dB SNR is achieved. The client is given a sheet with the ten sentences and has to respond with the corresponding number of the sentence heard. A percentage score is derived for each condition. For the FM system, the device is connected to the hearing aids and the microphone is placed approximately 15 cm from the speaker. While there certainly is debate on the particular demonstration method, it does offer a quick method to demonstrate the utility of such devices in approximately ten minutes.
An ever-growing group of clients that receive limited attention for their communication issues are those with mild traumatic brain injury. Investigations of individuals with mild traumatic brain injury have detailed significant issues with balance, vision, cognition and emotional consequences.47 Interestingly, the impact on the auditory system has all but been ignored by the medical profession, leaving clients to suffer with their communication issues. Bergemalm and Lyxell reported that clients 58% of clients were found to have auditory processing deficits following a mild traumatic brain injury and can have auditory processing issues 7–11 years post incident.48 Noel reported that a cohort of clients reporting mild traumatic brain injury,49 70% met the criteria for auditory processing as per Canadian guidelines.50 Further, 90% of those clients had normal peripheral hearing. Remediation of auditory processing disorders often focuses on environmental modifications, auditory training and compensatory strategies, and can encompass the use of assistive technology,51 although the use of assistive technology has focused on largely on children. Individuals suffering from mild traumatic brain injury represent an interesting cohort as they often are looking to maximize their potential and often want to get back to pre-injury functional level, therefore motivation remains high.
The following two cases demonstrate the usefulness of Jerger’s method in a client centred approach in treating clients with mild traumatic brain injury.
Case 1
This client had considerable issues with hearing and balance sustained from a motor vehicle accident (MVA) sustained four years prior to audiological evaluation. Prior to his accident he was a successful business man within the community growing a successful company. Since his accident he was unable able to return to work. The client thought it was a minor accident, however he could not recall driving home and was very confused and disorientated when he arrived home. Subsequently, he developed headaches and light sensitivities as well as balance issues and possible neurogenic stuttering. He was attending a brain injury program but was not referred for audiological or balance testing until his wife began searching for help. Peripheral hearing was found to be flat, mild sensorineural hearing loss with absent otoacoustic emissions (OAEs). Advanced testing demonstrated significant speech understanding difficulties in noise, with severe deficits for Words in Noise (WIN) test and left ear deficit on dichotic digits. His auditory brainstem response was abnormal for both ears with extended absolute and inter-peak latencies, as well as having abnormal auditory middle latency (C4 electrode effect) and extended P2 latencies across all sites (C3 and C4). No P300 could be elicited. Communication issues were so debilitating that client withdrew socially and this placed undue hardship on his family and severely limited social interactions. His main communication goal was to start enjoying family gatherings and going to social events with his wife however, he was ambivalent about hearing aids. Demonstration hearing aids and assistive technology (Phonak aids and compilot) was provided and the client was tested in a variety of listening situations. Data verified that the devices significantly improved communication especially in noise.
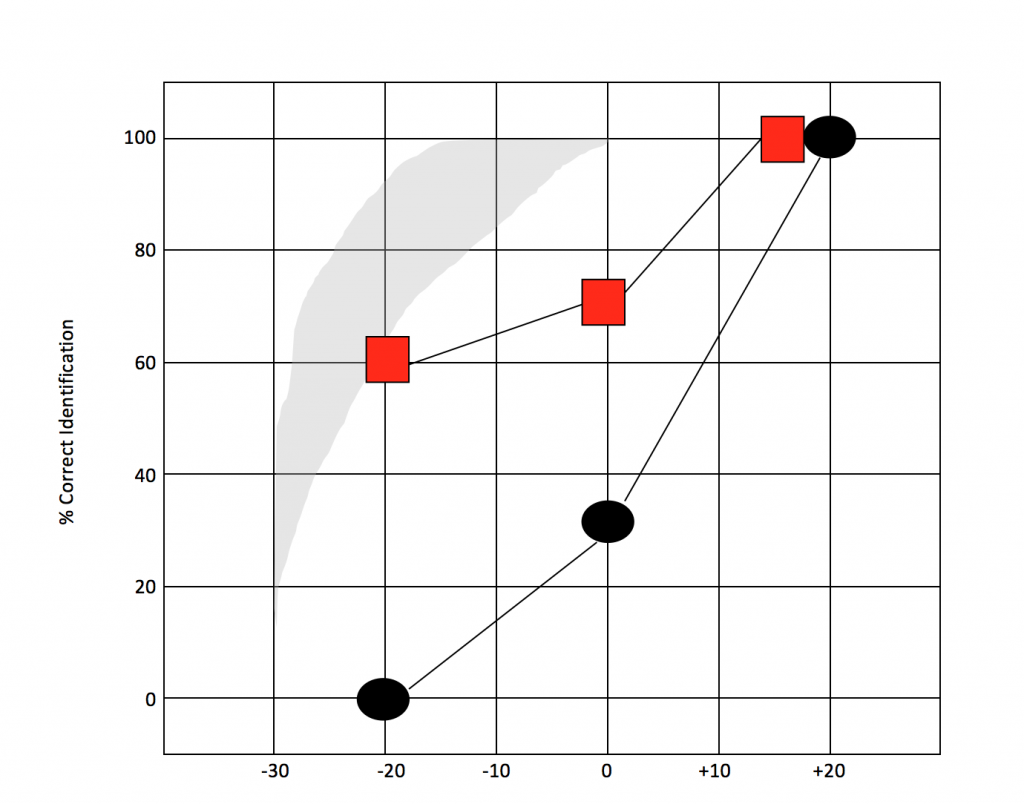
Figure 1. Demonstration soundfield testing for case 1 using SSI materials in three listening conditions, +20 db S/N ratio (easy), 0 db S/N ratio (average) and -20 dB S/N (very difficult) with hearing aids and assistive device (red square) and without devices (black circle). Adapted from Jerger and Hayes.45
Prior to beginning the session the client was asked to rank his communication difficulty, he noted that on a 10 point scale, he judged it to be 9 out of 10, demonstrating significant difficulty. After the 10-minute demonstration he noted the communication difficulty dropped to a 4–5. The client was referred to private practice to purchase devices. With the use of the devices, the client is now returning slowly to small social gatherings.
Case 2
MM was seen for testing after sustaining a concussion in an MVA approximately 2 months prior. No previous auditory issues were noticed prior to the accident. This client was a high achiever, being a health care provider, in which she held a public job, operated a successful private practice while working on her PhD. The client did not lose consciousness and noted difficulty hearing in noisy or less than ideal acoustic environments (home, restaurants, supermarkets, coffee house). Behavioural data indicated normal hearing sensitivity bilaterally but with reduced otoacoustic emissions. Moderate deficit on WIN and severe deficits bilaterally on compressed speech with reverberation. Electrophysiological evidence revealed a normal diagnostic ABR while it was difficult to obtain synchronous threshold data for the right ear, abnormal MLR, largely normal late latency response and absent auditory P300. Due to the audiological findings normal hearing sensitivity, reduced hair cell integrity, behavioural and evoked findings, the client was asked about her communication goals. Her top goal was to hear better in noise. There was a discussion on auditory training; the client was keen to try anything that would assist her on her recovery journey. Other health related issues (headaches, visual., fatigue) kept client from performing online auditory training however the client did obtain two Phonak aids and FM system (Rogers Pen). The hearing devices were fit by a private practice audiologist. Validation of the devices in the sound booth revealed significant benefit for the client. Testing was conducted without the aids, with the hearing aids and combination of hearing aids and FM system.
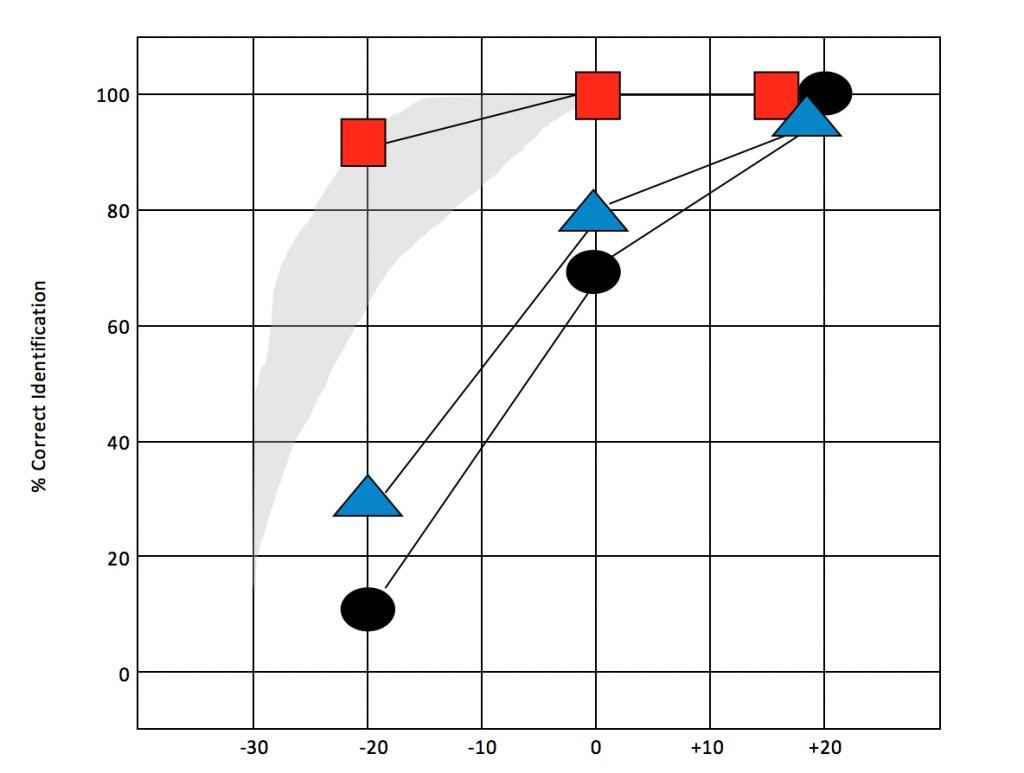
Figure 2. Demonstration soundfield testing for case 2 using SSI materials in three listening conditions, +20 db S/N ratio (easy), 0 db S/N ratio (average) and -20 dB S/N (very difficult) with hearing aids and assistive device (red square), with hearing aids only (blue triangle), and without devices (black circle). Adapted from Jerger and Hayes.45
The client consistently wore the devices constantly before returning for a recheck two months later. MM noted that the devices were supplying great support and she was able to socialize and family communication was easier. Behavioural data indicated a slight improved behavioural change however the auditory middle latency responses demonstrated 50% increase in the left ear for Na-Pa complex.
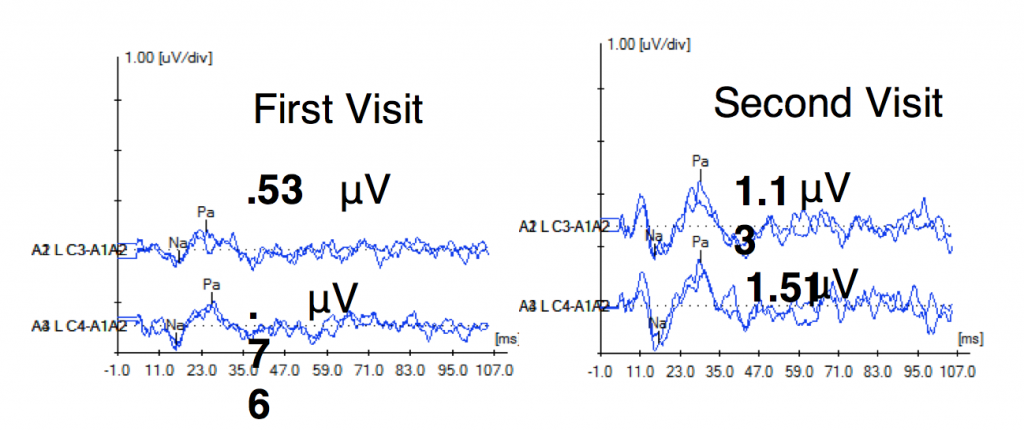
Figure 3. First visit. Auditory middle latency response (AMLR) for case 2 during initial audiological evaluation. Second Visit. AMLR for client 2 months after wearing hearing aids and assistive listening device consistently. Note improvement in amplitude (50%) after device use second visit.
Previous research has shown that FM system use can positively impact evoked potentials.52–54 It has been suggested that evoked potentials can be used as an outcome measure to monitor disease progress or rehabilitative improvement.55,56 Tremblay et al., demonstrated that changes in evoked potentials can be seen following the first day of training.39 There is literature to support the notion that improved clarity in the signal afforded by assistive technology may drive plasticity.54
This case was further complicated by legal and insurance issues and neither was willing to pay for the devices. The ten minute demonstration allowed the audiologist to provide functional benefit by providing a comparison of unaided, aided and combined (hearing aid and FM) conditions which clearly showed (1), that hearing aids alone do offer benefits and (2), the added benefit of combined use of low gain hearing aids with FM systems provided the best outcomes. The data was helpful in this case and the client was remunerated for complete costs of the devices. The client continues to improve and is ready to start to reinitiate her PhD studies.
As our profession continues to grow it is imperative that as clinicians we continue to change our clinical practices in order to meet the listening challenges of our clients. There is an art and science in the provision of audiological care. Engaging clients and evidence-based practice both require accountability and transparency to the clients and families, third party payers and society. In demystifying the issues around assistive listening technology directly with the client, the demonstration can have a positive impact. Enacting accessibility legislation across Canada will likely accelerate the integration of assistive listening devices into the mainstream and that can only be a good thing for clients who struggle with hearing difficulties. Let’s hope we are ready to facilitate that change.
Portions of this paper were presented at Canadian Academy of Audiology, Niagara Falls, Ontario, 2018, and IBIA World Congress, April 2019.
References
- Goldsmith M. Discord: The Story of Noise. Oxford: Oxford University Press; 2012.
- Carhart R.Test for the selection of hearing aids. Laryngoscope 1946;56:780–94.
- Bentler R, Niebuhr, Getta, and Anderson. Longitudinal study of hearing aid effectiveness. II: Subjective measures. J Speech Hear Res 1993;36:820–31.
- Humes, Halling, & Coughlin. Reliability and stability of various hearing aid outcome measures in a group of elderly hearing aid wearers. J Speech Language Hear Res 1996;39:923–35.
- Nabelek, Tucker, & Letowski. Toleration of background noises: Relationship with patterns of hearing aid use by elderly persons. J Speech Hearing Res 1991;34:679–85.
- Taylor and Bernstein. The Red Flag Matrix Hearing Aid Counseling Tool. Audiology Online, Article 816. Retrieved from http://www.audiologyonline.com
- Schuknecht Pathology of the ear. Cambridge: Harvard University Press; 1974.
- Musiek, Baran & Pinheiro. Neuroaudiology: Case Studies. Singular Publishing Group. San Diego; 1994.
- Bamiou, Free, Sisodiya, et al. Auditory interhemispheric transfer deficits, hearing difficulties, and brain magnetic resonance imaging abnormalities in children with congenital aniridia due to PAX6 mutations. Arch Pediatr Adolesc Med 2007; May;161(5):463–9.
- Bamiou et al. The role of the interhemispheric pathway in hearing. Brain Res Rev 1997;5-6:170–82.
- Bamiou et al. Auditory temporal processing deficits in patients with insular stroke. Neurology 2006;67(4):614–9.
- Giraud, Garnier, Micheyl, Lina, Chays and Chéry-Croze. Auditory efferents involved in speech-in noise intelligibility. NeuroReport 1997;8, 1779–83.
- May, Budelis & Niparko Behavioral Studies of the Olivocochlear Efferent System Learning to Listen in Noise. Arch Otolaryngol Head Neck Surg 2004;2004:660–64.
- Musiek F. Neuroanatomy, neurophysiology, and central auditory assessment. Part III: corpus callosum and efferent pathways. Ear Hear 1986;7(6):349–58.
- Kujawa S, Liberman MC. Hidden hearing loss—The problem and the promise. Association for Research in Otolaryngology. Available at: https://www.aro.org/page/KujawaLiberman
- Saunders GH, Haggard MP. The clinical assessment of obscure auditory dysfunction—1. Auditory and psychological factors. Ear Hear 1989;10(3):200–208.
- Tremblay, Pinto, Fischer, et al. Self-reported hearing difficulties among adults with normal audiograms: The Beaver Dam Offspring Study. Ear Hear 2015;36(6):e290–99.
- Ricketts and Hornsby. sound quality measures for speech in noise through a commercial hearing aid implementing digital noise reduction. J Am Acad Audiol 2005;16(5):270–77.
- Bradley and Sato. The intelligibility of speech in elementary school classrooms. J Acoust Soc Am 2008;123(4):2078–86.
- Ross, Brackett D, and Maxon A. Assessment and Management of Mainstreamed Hearing Impaired Children: Principles and Practices. Austin, TX: Pro-Ed Inc; 1991.
- Lewis et al. Speech perception in noise: directional microphones versus frequency modulation systems. J Am Acad Audiol 2004;15:426439.
- Valente, Fabry and Potts. Recognition of Speech in Noise with Hearing Aids Using Dual Microphones. J Am Acad Audiol 1995;6:440–49.
- Roup, Post, and Lewis. Mild-gain hearing aids as a treatment for adults with self-reported hearing difficulties. J Am Acad Audiol 2018;29:477–94.
- Jerger, Chmiel, Florin, Pirozzolo, and Wilson. Comparison of conventional amplification and an assistive listening device in elderly persons. Ear Hear 1996;17(6):490–504.
- Kochkin S. MarkeTrak VII: Customer satisfaction with hearing instruments in the digital age. Hearing J 2005;58(9):30–43 doi: 10.1097/01.HJ.0000286545.33961.e7
- Emmett and Francis. The socioeconomic impact of hearing loss in U.S. adults. Otol Neurotol 2015 Mar;36(3):545–50. doi: 10.1097/MAO.0000000000000562.
- Meinzen-Derr, Lim, Choo, Buyniski, and Wiley. Pediatric hearing impairment caregiver experience: impact of duration of hearing loss on parental stress. Int J Pediatr Otorhinolaryngol 2008 Nov;72(11):1693–703. doi: 10.1016/j.ijporl.2008.08.005.
- Duthey. A public health approach to innovation. update on 2004 background paper background paper. 6.21 Hearing Loss 2013.
- O’Neill, Lamb, and Archbold. Cost implications for changing candidacy or access to service within a publicly funded healthcare system? Cochlear Impl Internat 2016;17(sup1):31–35
- Shield B, ‘Evaluation of the social and economic costs of hearing impairment’. A report for Hear-It AISBL; 2006.
- Weinstein. Screening for otologic functional impairments in the elderly: whose job is it anyway? Audiol Res 2011 Mar 9;1(1):e12. doi: 10.4081/audiores.2011.e12.
- Lin, Metter, O’Brien, Resnick, Zonderman, and Ferrucci. Hearing loss and incident dementia. Arch Neurol 2011;68(2):214–20.
- Lin, Yaffe, Xia, Xue, Harris, Purchase-Helzner, et al. Hearing loss and cognitive decline in older adults. JAMA Intern Med 2013;173.
- Bamiou et al. Patient-reported auditory functions after stroke of the central auditory pathway 2012;43:1285–89.
- Kochkin S. MarkeTrak VIII: 25-year trends in the hearing health market. Hear Rev 2009;16(11):12–31.
- Grenness et al. Patient-centred care: A review for rehabilitative audiologists, Int J Audiol 2014;53:(sup1)S60–S67, DOI: 10.3109/14992027.2013.847286.
- Fielding, Teutsch, Breslow. A framework for public health in the United States. Pub Health Rev 2010;32(1):174–89.
- Kindig, Stoddart. Models for population health: what is population health? Am J Pub Health 2003;93:380–83.
- Reavis, Tremblay, and Saunders. How can public health approaches and perspectives advance hearing health care? Ear Hear 2016;37(4):376–80. doi:10.1097/AUD.0000000000000321.
- Tremblay K, et al. The time course of auditory perceptual learing:neurophysiological changes during speech sound training. Neuroreport. 1998 Nov 16;9(16):3557–60.
- Richards et al. Let the patient revolution begin. BMJ 2013;346:f2614. doi:10.1136/bmj.f2614.
- Sweetow R. Instead of a hearing aid evaluation, let's assess functional communication ability. Hear J 2007;60(9):26–31.
- Westfall et al. Practice based research – “Blue Highways” on the NIH roadmap. JAMA 2007;297(4):403–406.
- Deming. Out of the Crisis. Cambridge, MA: Massachusetts Institute of Technology Centre for Advanced Engineering Study xiii,1991;507; 1986.
- Taylor et al. Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Quality and Safety 2004;23(4):290–98.
- Jerger and Hayes. Hearing aid evaluation:clinical experience with a new philosophy. Arch Otolarygngol 1976;102(4):214–25.
- Speaks and Jerger. Method for measurement of speech identification. JSHR 1965;8(2):185–94.
- Hoffer and Balaban. Neurosensory disorders in mild traumatic brain injury. San Diego, CA, Academic Press; 2019.
- Bergemalm and Lyxell. Appearances are deceptive? Long-term cognitive and central auditory sequelae from closed head injury. Int J Audiol 2005;44:39–49.
- Noel G. Concussion and its impact on the auditory system. Poster presentation CAA October 2018, Niagara Falls, Canada; 2019.
- CSGSLPA. Guidelines on Auditory Processing Disorder in Children and Adults. Available at: http://sacoac.ca/sites/default/files/resources/Canadian-Guidelines-on-Auditory-Processing-Disorder-in-Children-and-Adults-English- 2012.pdf, 2012.
- Bellis T. Central Auditory Processing Disorders. San Diego: Singular; 1996.
- Hornickel, Zecker, Bradlow, and Kraus. Assistive Listening devices drive neuroplasticity in children with dyslexia. PANS 2012;109(41);16731–36.
- Johnston, John, Kriesman, Hall, and Crandall. Multiple benefits of personal FM system use by children with auditory processing disorder. IJA 2009;48:371–83.
- Keith and Purdy. Assistive and therapeutic effects of amplification for auditory processing disorder. Semin Hear 2014;35(1):27–38
- Harris and Hall. Feasibility of auditory event-related potential measurement in brain injury rehabilitation. Ear Hear 1990;11(5);340–50.
- Musiek F, Baran, and Shinn. Assessment and remediation of an auditory processing disorder associated with head trauma. J Am Acad Audiol 2004;15:117–32;117–32.

