Ototoxicity and Vestibular Dysfunction
Striking the Right Balance
Michael Vekasi, AuD, R.Aud, Aud(C), FAAA and Erica Zaia are coordinating the “Striking the Right Balance,” column which will cover the latest information on “all things vestibular.”
In this edition of “Striking the Right Balance,” Dr. Darren Tse, founder of the Ottawa Hospital Multidisciplinary Dizziness Clinic, discusses how to diagnose, prevent, and treat ototoxicity.
If you are a health care professional and would like to be more involved in all things vestibular, please sign-up for the Vestibular Special Interest Group. Sign-up by emailing JanineAllison.Verge@nshealth.ca to let us know you want to be included. Also, check out our Facebook page for a free list of online vestibular resources at the CAA National Vestibular Special Interest Group page.
Ototoxicity refers to damage to the inner ear due to exposure to noxious stimuli or medications. This can involve damage to the cochlea (causing hearing loss), the vestibular organs (causing dizziness), or both. Most commonly, ototoxicity occurs as a result of specific medications that damage the hair cells of the cochlea and vestibular system. These medications include things like platinum-based chemotherapeutics (e.g, cisplatin, carboplatin), and aminoglycoside antibiotics (e.g., gentamicin, tobramycin). Some patients are more susceptible to developing ototoxicity with these medication exposures, especially if they have genetic risk factors, or if they receive more than one medication at a time. Ototoxicity can cause permanent damage to the hearing and balance systems of these patients and the consequences can be quite devastating and disabling.
Vestibular ototoxicity can result in severe dizziness, vertigo, and oscillopsia (a visual bouncing of the visual surround when moving). The balance system relies on the vestibular system to detect angular and translational acceleration. When both vestibular systems are damaged by ototoxicity, the patient can become extremely dizzy and develop over-reliance on visual and proprioceptive cues to maintain balance. As a result, their balance is often extremely poor with eyes open, and virtually non-existent in the dark or with eyes closed. Additionally, the slightest turn of the head or shift in body position can cause overwhelming dizziness.
A Case of Vestibular Ototoxicity
Ms NM is a 45-year-old patient who presented with a 3-month history of disabling dizziness. She had undergone a gynecologic surgical procedure 3 months earlier and as a routine pre-operative precaution, she had been given a single dose of intravenous gentamicin, which is an aminoglycoside antibiotic. She spent a few days recovering from her surgery in the hospital, during which time she received 2 more doses of gentamicin post-operatively. She soon began to feel quite dizzy, describing a sensation of spinning constantly as well as visual blurring whenever she tried to move her head or change positions. By the time she came to see me 3 months later, she had become housebound and was using a walker to do even the simplest of activities.
On examination, Ms NM was very unsteady on walking, even with the walker. With her eyes closed, she could not maintain any semblance of upright posture. She had no spontaneous nystagmus, and her hearing was normal. She had large overt re-fixation saccades when performing head impulse testing on both sides. She also had a 6 line loss on dynamic visual acuity testing.
How to Diagnose Vestibular Ototoxicity
There is no test that can confirm ototoxicity. A good history of exposure to a potentially ototoxic medication, coupled with a temporal link between administration and onset of symptoms, is the key. The patient will typically complain of dizziness made worse with any kind of head movements, positional changes, and in situations where vision is limited (eyes closed, at night, in the dark, etc.). They may complain of oscillopsia, which is a bouncing of the visual environment on walking or head movements. And, they may have hearing loss and tinnitus as well if they suffered cochlear toxicity. The examination may be quite normal, but they usually exhibit a drop in their visual acuity on dynamic testing and often have overt re-fixation saccades on bedside head impulse testing. If they suffered cochlear toxicity, they may have abnormal findings on audiology.
Traditionally, video nystagmography (VNG) and rotary chair testing have been used to confirm bilateral vestibular hypofunction from ototoxicity. The VNG may show a bilateral caloric weakness, and rotary chair testing may show that there are reduced gains and abnormal phase. It is important to note that this does not really give you a good idea of how much functional impairment the patient has nor how each ear compares to the other. Finally, patients with bilateral vestibular hypofunction frequently find VNG and rotary chair testing very hard to tolerate, with some patients being unable to complete the testing.
We now have more direct tests of vestibular function that are useful in confirming ototoxicity. A Video Head Impulse Test (vHIT) can be very useful to confirm vestibulo-ocular reflex (VOR) dysfunction on each side independently. Figure 1 shows the vHIT results for Ms. NM. This test is very well tolerated, portable, and easy to perform, even in the patients with significant dizziness. If you have access to vHIT, I would recommend using it as your first-line test to confirm bilateral vestibular toxicity.
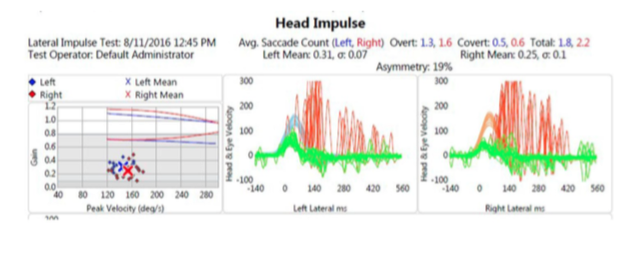
Figure 1. Lateral vHIT testing shows multiple bilateral overt saccades and severely decreased VOR gains.
(Ed note: for more information on vHIT, please read the feature article in our last issue.)
How to Prevent Vestibular Ototoxicity
First and foremost, try to avoid medications with known toxic profiles. Almost always there is a good non-toxic alternative that can be used. We know there are risk factors that contribute to developing ototoxicity (for example, duration of exposure, concomitant use other ototoxic medications, and some genetic factors), so be especially wary about using toxic medications in these patients. If it cannot be avoided, then monitoring of cochlear and vestibular function can be used, and the choice made to stop the medication if toxicity appears. For the vestibular side, use of vHIT is easily done even on a daily basis to monitor VOR function as a surrogate marker of vestibular function. A daily VNG would be much less reasonable, both for the patient, and the system. Audiology can be used to monitor hearing function.
How to Treat Vestibular Ototoxicity
Unfortunately, there is no way that the patient will regain their lost vestibular function. It is up to the brain to learn to compensate for this deficit using vision, proprioception, and other adaptive mechanisms. As such, the most effective therapy for ototoxicity is vestibular rehabilitation therapy (VRT). Patients will often make marked improvement in overall balance function with good VRT aimed at improving habituation, substitution, and adaption.

