Other People’s Ideas
Other People's Ideas
Calvin Staples, MSc, will be selecting some of the more interesting blogs from HearingHealthMatters.org which now has almost a half a million hits each month. This blog is the most well read and best respected in the hearing health care industry and Calvin will make a regular selection of some of the best entries for his column, Other People’s Ideas.
About a year ago, I provide a submission to www.CanadianAudiologist.ca looking at the impact of noise and the decibel. Last week, my colleague at work mentioned that he was at the Blue Jays playoff game and during one of the louder moments he decided to get an estimate of how loud it was inside the Dome with an App on his phone. His comment to me was simply "it was loud", but he could not believe how loud. His comments got me thinking about patients with NIHL and the shape of the NIHL audiogram. I have had this question several times over my career and often struggle with a tidy answer. Below are two blogs that help and a few more on NIHL.
NIHL-Shape Of The Audiogram – Part 1
Originally posted at HHTM On October, 2015. Reprinted with permission.
From time to time, I am asked either by a referring physician, a union, or a local Workers Compensation Board (sometimes referred to as the Worker’s Safety and Insurance Board) whether a particular worker has a hearing loss that could have been caused by his or her occupational noise (or music) exposure.
As a field of hearing health care professionals, clinically we make several assumptions about the nature of what a noise (or music) induced hearing loss would look like. This includes the “shape” or the slope of the audiogram (part 2 of this blog series), the degree and type of hearing loss, and the “correction” if any, for age (part 3 of this blog series). Because of the importance that “shape of the audiogram” seems to have in the acceptance or rejection of a claim for NIHL, as well as the “correction factor” that is applied to account for presbycusis, these two “assumptions” will be handled separately over the next several weeks (in part 2 and part 3 respectively).
Unlike most other areas of the field of audiology, very little modern research has been performed that underlies the auditory basis of noise exposure that leads to hearing loss. Much of the “seminal” research is from the 1970s and one has to be concerned about research that is more than 35 years old. Nevertheless a review of what our audiology ancestors found may provide a glimpse into why things are the way they are now.
85 dBA fence:
We have all heard of the 85 dBA “fence”. The way that it is used with noise induced hearing loss (and in many jurisdictions, music induced hearing loss) this fence or “threshold limit value” (TLV) is the action point- exposure below 85 dBA and no action is taken; at, and above 85 dBA and action is taken.
In 1966, the Committee on Hearing and Bioacoustics (CHABA) was the first North American group to try to get a handle on how some aspects of noise could affect hearing. Because it was among the first group of researchers to broach this complex topic, CHABA made some assumptions- some were not very important such as the relationship between temporary threshold shift (TTS) and permanent threshold shift (PTS), and other assumptions were of greater importance, such as whether intermittent noise exposure can be used to calculate an “equivalent” steady state type of noise exposure.
The CHABA recommendations were used by the United States Air Force to develop an enforceable hearing conservation program and that was first instituted in 1956. For an excellent overview of the history of this work, Dr. Alice Suter wrote a chapter in David Lipscomb’s excellent textbook Hearing Conservation in Industry, Schools and the Military (1994, Singular Publishing Group, ISBN 1-56593-380-X). This is the blue colored book that many of us have sitting on our bookshelves. Despite the age of this book, it is a gem and worthwhile getting if you can find it in a used book store.
In 1969, based on the earlier work of CHABA, in an attempt to develop a threshold limit value or fence to the general, non-military workforce, several groups, but mainly the American Conference of Governmental Industrial Hygienists (ACGIH) developed a voluntary standard that was later adopted by the Occupational Safety and Health Administration (OSHA) under the Walsh-Healy Public Contracts Act. This was initially only applicable to the contracts from the American government but later was also applied to Federal Coal Mine Health and Safety Act. And in 1971 this was extended through OSHA to the general American workforce (industry and construction). The Fence or threshold limit value was 90 dBA (over an 8 hour work shift and using a 5 dB exchange rate- see part 2 of this blog series).
In 1983 OSHA, recognizing that long term exposure to levels slightly below 90 dBA can also cause hearing loss, made an change called the Hearing Conservation Amendment which requires most, but not all workers, to have a baseline audiogram, annual audiometric test, and if the exposure is between 85 dBA and 90 dBA, be offered hearing protection.
Shortly after its creation in 1971, the National Institute for Occupational Safety and Health (NIOSH), in an attempt to establish best practice exposure limits, came out with a 85 dBA fence in 1972 (but still using the OSHA and CHABA 5 dB exchange rate). In 1998, NIOSH revised its recommendations by using a 3 dB exchange rate, while still maintaining the 85 dBA threshold limit value fence.
Most countries outside of the United States follow the NIOSH 85 dBA threshold limit value with a 3 dB exchange rate and this includes the European Union, and most provinces in Canada (with the exception of Quebec). Of notable exceptions around the world are Brazil and Israel that still use the more conservative OSHA recommendations.
NIHL-Shape of the Audiogram – Part 2
Originally posted at HHTM On October 13, 2015. Reprinted with permission.
The “shape” or configuration of the sensori-neural hearing loss, at least in worker’s compensation board claims for noise exposure, is one of the base elements for deciding whether a hearing loss is indeed a noise induced hearing loss. Yet, not all audiograms of workers exposed to high levels of noise (or music) have a “notched” audiogram with the greatest hearing loss being in the 3000-6000 Hz frequency region.
Dr. David Barrs, MD, who is now with the Mayo Clinic in Rochester, MN, did some interesting work earlier in his career. [2]. Barrs and his colleagues found that only 37% of those workers who were exposed to noise and had a sensori-neural hearing loss had an audiometric notch in the 3000-6000 Hz frequency region.
They attributed this to a number of potential reasons such as presbycusis which over time reduced the 6000 Hz and 8000 Hz acuity such that the upper frequency end of the notch was flattened out. Nevertheless, not having an audiometric notch does not prevent a diagnosis of noise exposure, and conversely, having an audiometric notch does not mean that the hearing loss was noise induced.
As we will see below, the studies about the various proposed reasons for why the greatest hearing loss is in the 3000-6000 Hz region reads as an historical novel with contributions from as far back as 1934.
Since these original studies (which were in some cases, mere opinion) a number of “position” papers and consensus group statements have been attempting to place these historical works in their proper current clinical contexts. Among others, these include ACOEM Guidance Statement for Occupational Hearing Loss, (2012) from the American College of Environmental Medicine. which stated, among other things, that the audiometric notch could vary depending on the spectrum of the noise source as well as the shape (but primarily the length) of the ear canal.
Another excellent review for those who are interested in further reading is an article entitled “5 Myths in Assessing NIHL” (from Audiologyonline.com). This article deals with, as the name suggests, 5 myths about NIHL and one of them is about the symmetrical versus asymmetrical shapes of the audiogram. This remains a highly contested area, not because there is debate on whether this actually occurs (it does) but how a worker who has an asymmetrical hearing loss should be compensated- should the better hearing thresholds be used, or some weighted combination of the two ears?
And finally, for those who are more interested in musicians, I have a nice review article about some of these issues, also at www.audiologyonline.com.
Here is a synopsis of the studies about the various potential reasons about the NIHL notch. Several explanations have been proposed for this audiometric notch over the past almost 80 years but to date, there is no one accepted explanation; it is a frequently observed audiometric shape (but not the only noise induced shape):
Crow, Guild, and Polvagat, 1934 have shown that part of the explanation may be related to a poorer blood supply in the cochlea that corresponds to the 3000-6000 Hz region;
Bohne, 1976 showed that there is a greater susceptibility for damage of the supporting structures of the cochlear hair cells in the 3000-6000 Hz region;
Hilding, 1953, and Schuknecht and Tonndorf, 1960 showed that the orientation of the stapes footplate in the middle ear, into the inner ear is such that the primary force vector aims towards those cochlear hair cells in the 3000-6000 Hz region, with the effect of eventual failure because of the constant hydro-mechanical action; and
Tonndorf, 1976, and Caiazzo and Tonndorf, 1977, have shown that permanent noise exposure has its greatest effect approximately one half octave above the peak frequency of the noise spectrum, and since the “peak” is typically that of an adult’s ear canal resonance (at 2700 Hz), the greatest hearing loss will be the 4000-6000 Hz region.
Despite the age of these references, there are no more modern data that contradict these findings or suppositions.
Footnote
Barrs, D., Althoff, L., Krueger, W., & Olsson, J. (1994). Work-related, noise induced hearing loss: Evaluation including evoked potential audiometry. Otolaryngology- Head and Neck Surgery, 110(2), 177-184.
NIHL- Age Corrections – Part 3
Originally posted at HHTM On October 20, 2015. Reprinted with permission.
In many state or provincial worker’s compensation boards there is a “correction factor” that may be applied to a calculated noise induced hearing loss. In many cases, this is a “presbycusic” correction and may amount to subtracting 0.5 dB off of the calculated average hearing loss for each year over the age of 60. On the surface, this appears to be an expeditious ”correction” factor; it is quick and easy to calculate and at least is in the ball park of a correction for age.
OSHA in the United States uses rather scary looking tables F-1 (for males) and F-2 (for females) that can be found in their optional appendix. This gives age corrections for ages starting as early as 23 (with a 1 dB correction given at both 4000 Hz and 6000 Hz). The corrections start to exceed 5 dB by age 32 with a slight correction also being given for 2000 Hz and 3000 Hz. It is slightly less dramatic for women in table F-2 with corrections on the order of 5 dB beginning at age 35 or 36. It is not known why there is a difference between men and women although there are many metabolic and hormonal theories being proposed.
At least for men, there is a 30 dB age correction at 6000 Hz and about a 28 dB one at 4000 Hz for those over the age of 60. There are no additional age corrections above age 60. For those who like numbers, part of table F-1 for men is given below. Unfortunately it’s still given below for those who don’t like numbers. (The actual table has entries for every age in 1 year units).
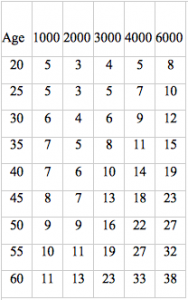 It is interesting to note that a slight hearing loss is “expected” for even 20 year olds. It is also important to recognize that OSHA is based on a 90 dBA fence and uses the 5 dB exchange rate which significantly underestimates the effect of noise (and music). Most jurisdictions in the world use criteria that are similar to those used by NIOSH (85 dBA action point and a 3 dB exchange rate).
It is interesting to note that a slight hearing loss is “expected” for even 20 year olds. It is also important to recognize that OSHA is based on a 90 dBA fence and uses the 5 dB exchange rate which significantly underestimates the effect of noise (and music). Most jurisdictions in the world use criteria that are similar to those used by NIOSH (85 dBA action point and a 3 dB exchange rate).
The “intent” of this table however was primarily to assist in determining there was actually a real hearing change (a change exceeding the Standard Threshold Shift) or whether it can be attributed to aging.
In the “subtract 0.5 dB for every year over the age of 60” scenario, this is something that may be a bit over-zealous. In this scenario, hearing loss due to noise exposure would be the average of several frequencies such as 500 Hz, 1000 Hz, 2000 Hz, and 3000 Hz, depending on the jurisdiction. A 0.5 dB/year correction (subtracted from the above four frequency average) would amount to a 2 dB change for each frequency for each year over 60, or equivalently, an 8 dB change for each year at 3000 Hz only. This is rather dramatic, since changes at 3000 Hz typically amount to one decibel at most/year. This is partly related to the fact that most hearing loss occurs in the higher frequency region such as 4000 Hz and 6000, and its progression experiences a toughening or slowing down of hearing loss over time (see blog on asymptotic hearing loss).
Although the references are dated, like most areas of what we know about noise exposure, Bies and Hansen, 1990, and Bies, 1994, criticized the 0.5 dB correction as being too over- zealous. It is really just a “correction” that saves money for the various compensation boards rather than having any clinical reality.
Another assumption behind this correction is that the effects of noise exposure and music exposure are the same animal. Research in this area is very difficult to perform but a 2000 article in Hearing Research by Gates, Schmid, Kujawa, Nam, and D’Agostino suggests that even presbycusis and noise exposure are quite different in their progressions and underlying structures. This doesn’t answer the question of music exposure versus noise exposure but does bring up the point that sensori-neural hearing loss may be quite different depending on the source, despite audiometrically appearing to be quite similar.
The Gates, Schmid, Kujawa, Nam, and D’Agostino article is so important (even though it is also 15 years old) that a future blog will be dedicated to this…. in fact, stay tuned for next week!
Phase 3 Drug Study for Noise induced Hearing Loss Cure
Originally posted at HHTM On September 29, 2015. Reprinted with permission.
Two and a half years ago Hearing International discussed various homeopathic medicine treatments for In Part V of this discussion, we referenced theimpressive a research headed by Dr. Kathleen Campbell, audiologist and researcher at Southern Illinois University. A prolific researcher, whose team at Southern Illinois University has discovered that antioxidants can reduce hearing loss created by aminoglycocide ototoxicity and reduce or eliminate the effects of noise induced hearing loss.
At the beginning Phase 2 of US Food and Drug Administration (FDA ) clinical trials in the use of D-Methionine (D-Met), Dr. Campbell indicated that the goal of their team was to be sure that when they “came out with a statement, it is scientifically correct and well documented.” In an interview with Beck (2013), she underscored that point as she presented that there are thousands of supplements, vitamins and other “cures” available from the Internet and other sources that have very suspicious claims as to their benefit.
The Science Behind the Research
In our last discussion of this topic, Mandal (2013) described the science involved as related to oxygen in that “all living organisms use oxygen to metabolize and use the dietary nutrients in order to produce energy for survival. (Click here for an antioxidant video). Oxygen is a highly reactive atom that is capable of becoming part of potentially damaging molecules commonly called “free radicals.” If not familiar with the relationship of oxidation of molecules into free radicals and how antioxidants can affect metabolism, a super discussion is available at Healthy Check (2015). Basically, due to metabolism and other factors, such as noise exposure the auditory system, unstable molecules are created in the cellular structure by “oxidation”. In the auditory system, theory has it that these unstable, oxidized molecules or “free radicals” attack other portions of the cellular structure to steal electrons to become stable again. This stealing of electrons from other molecules causes a less stable cellular structure and, in the auditory system, contributes to the loss of hearing sensitivity. This process also is also thought to be a cause of other disorders such as heart disease, cancer, aging and many other conditions.
A stabilizing factor for these unstable molecules is antioxidants. Antioxidants serve as a stabilizing agent by reversing the oxidation process as they donate their atomic structure to the oxidized molecule (free radical). These antioxidants are a source of controlling these free radicals as they have extra electrons that can turn the free radical molecule back into a healthy molecule by donating one of its electrons to the free radical. This process does not turn the antioxidant into a free radical as they have electrons to spare and are not disturbed by this structural modification. Some antioxidants are created by the body naturally while other are obtained from the food we eat. Vitamin supplements often include antioxidant vitamins such as C and E to offset these molecular oxidation issues controlling the free radicals but can also be found in fruits, vegetables, wine, chocolate, and many other foods that we eat everyday. D-Met, the substance that is being tested as a drug to replenish these electrons to the free radicals within the auditory system is an antioxidant that has been scientifically proven to reduce the oxidation of molecules (or creation of free radicals) in the auditory system and the chain reaction that causes damage to hearing.
Proven to Date
Dr. Campbell’s team, collaborated by other research teams, have now proven that:
- D-met protects against radiation-induced oral mucositis, cisplatin-induced ototoxicity and other cisplatin side effects, aminoglycoside-induced hearing loss, and noise-induced hearing loss.
- Phase 2 clinical trials for radiation-induced oral mucositis and cisplatin-induced hearing loss have shown significant protection with oral D-met administration.
- D-met also provides partial protection from aminoglycoside-induced hearing loss with no antimicrobial interference in animal studies.
- D-met protects against noise-induced hearing loss if given before, during or even when first started up to 7 hours after noise-cessation. It also protects if only given prior to the noise, even if stopped one day prior to the noise exposure.
The New Research
In August 2015, the research moved on to Phase 3 of the FDA clinical trial. Since the use of D-Methionine has been proven to be of benefit for noise induced hearing loss, the Phase 3 of the FDA process will establish the safety and the dosage of the drug for use in humans. Dr. Campbell’s team has now secured funding from the US Department of Defense and has begun Phase 3 of the FDA clinical trial at Fort Jackson ere volunteer subjects that are Army soldiers attending the Drill Sergeants Course are participating in the study. As part of their training over 11 days at the rifle range as the drill sergeant candidates, each will fire an M16 at least 500 times. The M16 is one of the U.S. Army’s quieter weapons, but that isn’t saying much. For the shooter, shots from the rifle, even if muffled by Army-issue earplugs, register above the noise level hearing experts consider safe. As audiologists know, the M-16 puts out an impulse noise of over 154 dB (A) well above the levels that will cause damage to the auditory system and another variable is the number of these exposures per day. Most audiologists realize that a day at the rifle range will cause a significant temporary threshold shift and some permanent auditory damage, making this environment perfect for this phase 3 trial of the D-Methionine therapy. After searching for 10 years, she found the Army where noise is part of everyday life, especially when spending lots of time at the rifle range. She and her two research nurses use a former break room at the Drill Sergeant Academy to administer hearing evaluations and necessary questionnaires to discuss about potential side effects, and administer the D-Met during Chow time.
According to the Army (2015), Staff Sgt. Tyler Durden of the Joint Readiness Training Center at Fort Polk, Louisiana, already experiences tinnitus, a ringing in the ears caused by hearing damage. He was a ready volunteer for the trials because “this is a huge opportunity to make things better for everybody” subject to hearing loss. He slugged back a dose of the orangish liquid, whose taste he said reminded him and other waggish Soldiers of the excretions of an animal none of them is likely to have encountered. Even so, Sgt. Durden did not request the proffered water, juice or peppermints nurses had brought with them to alleviate the taste of the medicine.
Since the study is randomized and double blind and the data will go to Yale for analysis, even Dr. Campbell does not know who gets the drug and who gets the placebo. This is a seminal moment for the cure of noise induced hearing loss. If it works, there will be substantially less hearing loss due to noise exposure… what will audiologists do!
References
Beck, D. (2013). Clinical Trials of D-Methionine: Interview with Kathleen Campbell, Ph.D., Interviews: September 13, 2013, American
Academy of Audiology. Retrieved September 29, 2015.
Mandal, A., (2013). What are antioxidants. News Medical. Retrieved September 29, 2015.
Marcus, A. (2015). Army tests hearing drug at rifle range. Wall Street Journal. amy.marcus@wsj.com Retrieved September 28, 2015:
Videos
Healthspan (2011). Understanding Antioxidants. Retrieved Septemeber 29, 2015.
Dangers of Hearing Loss from Earbud Use Highlighted on National TV
Originally posted at HHTM On September 24, 2015. Reprinted with permission.
 NEW YORK — NBC’s Today Show, a staple of morning television for more than 60 years, recently featured a segment on the increase in noise-induced hearing loss among children and young adults using earbuds.
NEW YORK — NBC’s Today Show, a staple of morning television for more than 60 years, recently featured a segment on the increase in noise-induced hearing loss among children and young adults using earbuds.
The segment mentioned a February, 2015 World Health Organization (WHO) warning that more than 1.1 billion teens and young adults are at-risk for permanent hearing loss due to portable stereo use and other forms of recreational noise exposure.
Testing for Safety
During the 4½ minute segment, several students agreed to have their listening levels measured while using portable listening devices (PLDs). Intensity levels tested ranged from safe (80 dBA for one user) to dangerous listening levels for all other PLD users (87 to 105 dBA). The students were then educated on levels that assured safe listening.
Dr. Brian Fligor and Dr. Sandra Levey conducted the research. Dr. Fligor has focused on noise-induced hearing loss (NIHL) and Dr. Levey, professor at Lehman College in the Department of Speech-Language-Hearing Sciences, has focused on the language effects of NIHL.
The listening levels of 189 PLD users on the Lehman College campus were measured prior to the NBC segment. They found 58% of the participants listened at dangerous levels (93 dBA).
The listening levels of 160 PLD users on the Lehman college campus and in Union Square in New York City were also measured. Similar results were obtained at both locations, with 62% listening at dangerous levels (95 dBA), both in the presence of loud traffic noise in the New York City location and in a context on a quiet campus.
In view of these findings, Dr. Levey emphasized, “The onset and progress of NIHL is insidious, with the listener unaware of the gradual loss of hearing abilities.”
Research Continues to Confirm Risk
The Today Show segment dovetails with an April, 2014 JASA[1] report that revealed nerve synapses may be more vulnerable to damage than hair cells within the inner ear[2].
In the JASA report, entitled Hidden hearing loss: Permanent cochlear-nerve degeneration after temporary noise-induced threshold shift, the authors[3] posit that primary neural degeneration has remained hidden for two reasons: (1) the spiral ganglion cells, the cochlear neural elements commonly assessed in studies of sensorineural hearing loss, survive for years despite loss of synaptic connection with hair cells, and (2) the degeneration is selective for cochlear-nerve fibers with high thresholds.
When young animals were exposed to loud noise, even just once, they had accelerated hearing loss later in life.
This report directly challenges the view that sensorineural hearing loss primarily targets hair cells alone, and that cochlear-nerve loss is secondary to hair cell degeneration. In their work, using guinea pigs and mice, noise exposure caused permanent loss of greater than 50% of cochlear-nerve/hair-cell synapses.
Their research suggests neural degeneration is an important contributor to the handicapping condition of sensorineural hearing loss, and noise exposure guidelines should be re-evaluated, as the traditional pure tone audiogram may not be the most sensitive measure of noise damage.
Footnotes
Journal of the Acoustical Society of America
Within the inner ear (cochlea), there are thousands of tiny sensory cells called stereocilia–hair cells. These hair cells change the acoustic vibrations into electrical signals which are then sent to the brain via the auditory nerve.↵
Drs. Charles Liberman and Sharon G. Kujawa of the Massachusetts Eye and Ear Infirmary

